One aspect of the federally-mandated changes in insurance coverage of birth control products hasn’t gotten nearly the attention it deserves.
The problem that reformers were addressing is that birth control prescriptions are expensive. It’s not just the $60 or $100/month for a pack of pills. There’s also the $60 or $100 for an appointment with a doctor, and the followup visits for prescription refills.
If birth control was safe enough to sell over the counter for a penny or a dime a pill like generic aspirin, there would be no controversy. Religious figures could continue their teachings about birth control (and NOT be expected to pay for it), and women would make their own choices about actions they think are right for them.
 Most people consider a good sex life an important part of living. While there are basically no consequences for men, the possibility of becoming pregnant is always a consideration for women. The modern world offers women the potential to cultivate other aspects of their lives than “Jane, mother of 8”. So even though the pills are expensive, and not entirely safe, millions of women around the world suck it up as the costs they must pay to have a good level of control over their uteruses, and also to hopefully enjoy the many advantages of having a good sex life.
Most people consider a good sex life an important part of living. While there are basically no consequences for men, the possibility of becoming pregnant is always a consideration for women. The modern world offers women the potential to cultivate other aspects of their lives than “Jane, mother of 8”. So even though the pills are expensive, and not entirely safe, millions of women around the world suck it up as the costs they must pay to have a good level of control over their uteruses, and also to hopefully enjoy the many advantages of having a good sex life.
To understand why birth control products are so expensive, and are still prescription-only, we need to consider how how The First Pill was originally developed.
In the 1930’s, biochemists found that the hormone Progesterone suppresses ovulation during pregnancy. The Corpus Luteum produces a large amount of progesterone after a follicle releases an egg. If the released egg is fertilized and implants in the uterus, a signal is sent to the Corpus Luteum to continue progesterone production. This continues until the placenta takes over Progesterone production later in the pregnancy.
If the signal is not received, the corpus luteum stops progesterone production. It is the sudden drop in progesterone levels that triggers menstruation.
In the early 1950’s, Harvard gynecologist John Rock was working with a group women who had trouble conceiving. He found that suppressing ovulation and maintaining a “pseudo-pregnancy” with supplemental progesterone and estrogen helped about 15% of those patients become pregnant.
But a large dose of progesterone didn’t suppress ovulation 15% of the time on the first cycle, and 300mg/day was a rather large amount of progesterone ($expensive$). The search for an ovulation-suppressing product for routine use moved to other chemicals (“Progestins”) that suppress ovulation sort of like human-Progesterone.
[BC researcher] Pincus asked his contacts at pharmaceutical companies to send him chemical compounds with progestogenic activity. Chang screened nearly 200 chemical compounds in animals and found the three most promising were Syntex’s norethindrone and Searle’s norethynodrel and norethandrolone.
–studies of progestins to suppress ovulation.
The first Birth Control Pill came out in 1957, and was approved for use as a contraceptive by the FDA in 1960. The first reports about blood clots in Pill users appeared in November 1961, 4 years after The Pill first entered the market. In 1970, Senator Nelson’s hearings resulted in package inserts about The Pill’s potential risks.
After about 60 years of research and development, there are now dozens of birth control pill fomulations. They all use one progestin or another to suppress ovulation. Combined oral contraceptives have estrogen too – this is usually the super-estrogen ethinyl estradiol.
Clotting problems are seemingly related to the amount of estrogen present. Modern birth control pills have 1/3 (or less) as much estrogen as the original Pill. But clotting is still a concern:
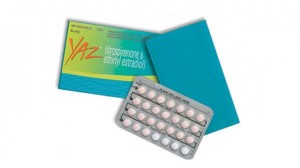 Women who take contraceptive pills containing drospirenone (active ingredient in Yaz) have a six- to sevenfold risk of developing thromboembolism compared to women who do not take any contraceptive pill, and twice the risk of women who take a contraceptive pill containing levonorgestrel.
Women who take contraceptive pills containing drospirenone (active ingredient in Yaz) have a six- to sevenfold risk of developing thromboembolism compared to women who do not take any contraceptive pill, and twice the risk of women who take a contraceptive pill containing levonorgestrel.
–http://en.wikipedia.org/wiki/Drospirenone#Adverse_effects (emphasis added)
A report on the Yaz Problem by ABC News last year says thousands of lawsuits have been filed.
Many women have to try several different brands before they find one with side effects they can tolerate. Others are happy with their pill-induced infertility after the 2-3 months it takes for their moods stabilize , only to find that their hair starts thinning/falling out after 2 years. Whoops.
Birth control pills are expensive to develop because they require massive amounts of research and experimentation to find new, patentable chemicals that suppress ovulation but are also not acutely toxic. The potential for side effects requires semi-regular visits with the prescribing physician.
If research does not result in a patentable substance, pharmaceutical companies would never recoup its investment.
The entire focus of the last 60 years of birth control research has been on expensive options that create a large financial return for the companies making the investment. As will be covered in my next post, this has resulted in all sorts of products with a single flaw that CANNOT be fixed.
To receive notification of this post, please sign up for the feed by putting your email address in the ‘feedburner’ box to the right.
There ARE some good options for safe, effective contraception, but this research will probably have to be publicly funded.
UPDATE – a followup has been posted: How Birth Control Torpedos Libido
Leave a Reply